by Heinz U. Lemke, PhD
Part 1 from the last issue is available here.
Part 2: Digital Operating Room (DOR) IT architectures for interoperability
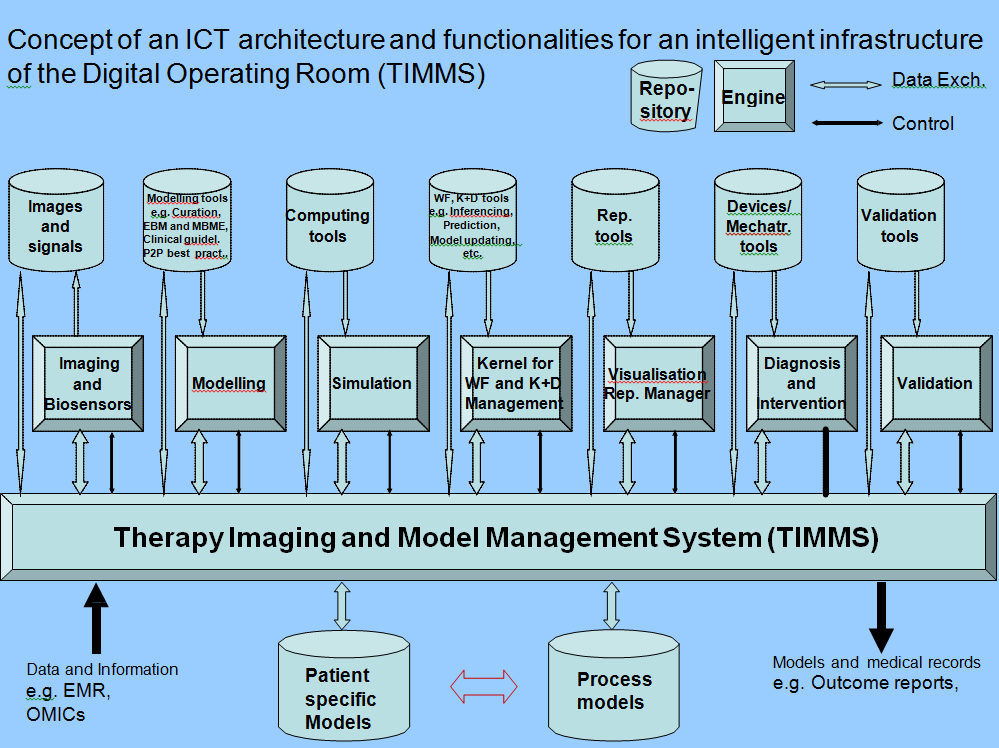
Architectural features, for example, as part of an intelligent infrastructure of an OR have only recently become a focus in discussions relating to interventional settings [1,4]. Such an IT reference architecture may be referred to as a Therapy Imaging and Model Management System (TIMMS) [4].
A TIMMS-like architecture and its application for achieving image and model guided therapy has been the subject of discussions in the DICOM and IHE standard activities. An implementation of a prototype based on open standards of the modular TIMMS-like architecture is in progress at the Innovation Centre Computer Assisted Surgery (ICCAS) in Leipzig, Germany. TIMMS is a comprehensive medical-surgical communication and assist system (Fig. 3), which is composed of interconnected computer hardware and software components (such as engines, repositories and an IT infrastructure).
There are seven TIMMS engines, which may be defined as software modules which can be executed on an appropriate computing machine in order to provide interventional functionalities. These engines relate to imaging and biosensor data acquisition, modeling, simulation, workflow and knowledge and decision management, visualization, intervention and validation. Some of these engines are already present and used in modern OR systems.
The Kernel for workflow and knowledge and decision management provides the strategic intelligence for therapeutic planning and workflow execution. Often this module (or parts thereof) is integrated into some of the other engines, as the need may have demanded. This important computing kernel (or “brain”) of the system may use different forms of logic, different database structuring, agents and other forms of artificial intelligence, depending on the specific applications of the performed procedure.
In a full realization, a TIMMS may provide the following features and functions throughout the course of a medical and surgical treatment:
- Standardized interfaces for communication and mechatronics, thereby creating a unified environment for the input and output of data (including the representative on and display of information and images, as well as the electromechanical control of surgical and navigational devices)
- Creation and maintenance of a Patient-Specific Model (PSM), thereby providing a multi-scalar, comprehensive, precise, personalized representation of the patient
- Creation and maintenance of a system for Process Modeling (PM) of all aspects of the surgical workflow, to ensure efficiency, learning and safety throughout operative procedures
- Real-time knowledge management and decision support system thereby promoting optimized diagnostic, prognostic and therapeutic decisions throughout the treatment workflow
- Validation and approval procedures, thereby providing quality assurance, patient safety, system security and processing of medical evidence towards securing better patient outcome.
Features 1, 2, 3 and 4 are the prerequisite of an intelligent infrastructure of an OR. A full realization of these functions is still a long way away. In practice, however, some small subsets of patient models, process models and/or real time knowledge management have been implemented and clinically tested. Feature 5 can begin to be properly addressed when features 1-4 have reached a tangible stage of implementation from which one can derive appropriate requirements for safety testing and feature/(usage) classification for devices and systems approval.
Feature 2 is subject to standard activities in working groups in DICOM and IHE in surgery. Feature 5 is of major concern in a number of regulation agencies such as FDA, PMDA, CEN and DIN. FDA and PMDA will be discussed further in section 4 below.
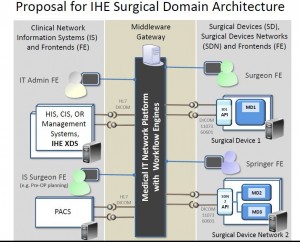
One of the architectures proposed in OR:NET [14] is somewhat different in appearance with respect to the TIMMS architecture but conceptually contains an equivalent base structure (see Fig 4).
References
[1] Goldman JM (2007): The OR of the Future: Current activities and Health IT implications, HIMSS07 New Orleans.
[4] Lemke HU, Vannier MW (2006): The operating room and the need for an IT infrastructure and standards. Editorial, International Journal of CARS, Vol 1, No 3, Springer Verlag, Heidelberg,Germany
[14] http://www.ornet.org
