source of the image: https://www.flickr.com/photos/brother-uk/31501281374
by Golafsoun Ameri
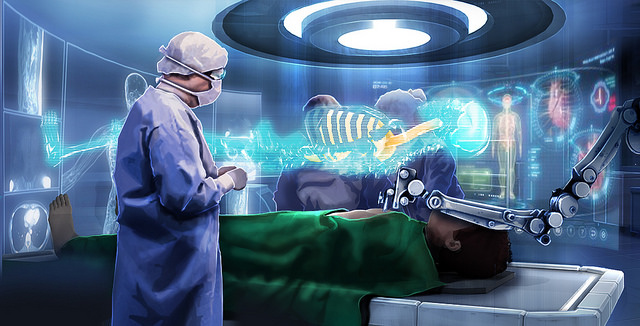
Given the growing interest in augmented reality image guidance systems, it is important for our community to discuss the best practices for the development of such tools, especially for improving implementation and clinical adoption. Other communities that develop similar tools, such as software engineering and game-based training, have a history of development best practices and guidelines that support optimal development. This article aims to describe and initiate discussion on multiple aspects of best practices for the development of augmented reality image guidance systems for surgical and therapeutic interventions.
Regulation
The life cycle of the development of medical software needs to meet certain regulatory requirements to obtain Health Canada or Food and Drug Administration approval for clinical trials and use in the clinic. International standards, including the International Electrotechnical Commission (IEC) 62304, have been developed to provide a framework for the development, maintenance, and evaluation of software. Their goal is to enhance the reliability and safety of the software for clinical use. In addition, software developed for clinical application must comply with other standards, including Quality Management Systems as described in International Organization for Standardization (ISO) 13485, and Risk Management Process as described in ISO 14971. These standards encourage developers to adopt rigorous processes and documentation for elements of requirements elicitation and product quality assurance prior to commencing implementation. The degree to which this limits the flexibility of the development process is an open question.
Clinical need and clinical input
It is known in the medical device industry that one of the major failure points for a product is related to the lack of a clinical need. The fate of an image guidance system is similarly dependent on the clinical need and how effectively it is addressed. It is essential that the clinical need is outlined, and the desired guidance system described, by clinical experts prior to the design and development of a guidance system. In addition to identifying the clinical need, clinician input is invaluable regarding identifying the environmental and practical limitations that must be considered during the design and development of a guidance system. It is important to note that clinicians with different levels of expertise and experience may view a clinical problem differently and envision different solutions. Therefore, it is important to involve as many clinicians as possible to elucidate alternatives for providing the most optimal guidance system.
Iterative and small-scale evaluation
While the initial design decisions may seem well-justified, especially after considering clinicians’ input, there is no substitute for iterative, small-scale evaluation of the system with the intended clinical users. Incremental evaluation which interrogates each design decision can better determine its effect on the goals of the guidance system. Special cases and considerations that can radically change the system for the better may also be unearthed. The importance of incremental evaluation, assessing each design decision and identifying special cases and considerations, cannot be overstated. This recommendation draws parallels with a methodology known in the larger software development community as agile development, which focuses on analyzing and improving the product throughout its development.
Trade-off between standardization and versatility
There is often a high degree of variability in the approaches taken by clinicians to perform any given procedure. Such variations may have roots in a lack of standardization for teaching and training, or each physician’s own experience of how to achieve optimal performance. Therefore, as a developer of a medical system, one must accept a certain fundamental choice between standardization and versatility. Either a system must support this variability and be versatile to fundamental variations in how the procedure is performed, or its use must be standardized and the standards explicitly stated in order to remove these variations. The choice between standardization and versatility should be made deliberately after the initial discussion with the intended user, i.e. the clinician, or discovered during iterative evaluation.
Multi-use system design
Image-guided interventions are composed of multiple tasks, including navigating surgical tools toward the region of interest and positioning them at the target. Therefore, navigation and positioning can be thought of as different uses of an image guidance system aimed to guide the entire set of procedures. Recognizing that such guidance systems are fundamentally multi-use has important implications on how they should be designed and their potential applications. For example, a guidance system has multiple parts that can be configured to accomplish different aspects of an image-guided procedure ranging from training to quality assurance (QA).
Training is an important part of any clinical procedure, and image-guided procedures are no exception. Configuring a guidance system to provide a training platform would be desirable, because clinicians would gain more experience with the system itself and would not be subject to minute differences between the training and clinical system that would cause undue distraction or cognitive load. One example could be configuring the guidance system to allow integration of synthetic images and models for training purposes. This would also have the added benefit of eliminating the need for physical phantoms, making the training platform more affordable and accessible.
Moreover, there has been a paradigm shift in medical education toward competency-based training, a by-product of which is the emphasis on individual and quantitative assessment of trainees. An image guidance system may be configured to provide quantitative skills assessment for QA. One example could be providing a procedure replay capability for retrospective quantitative analysis and assessment for QA. This could be achieved by simply recording the tracking information of the tracked intra-operative images and surgical tools.
The potential use of an image guidance system for multiple uses, other than surgical guidance, may not be clear to the collaborating clinicians initially. However, developers of such guidance systems, who have a better grasp of the capabilities of the technology, may need to envision and design additional functionalities for their guidance system first. This design can then be further refined and the usefulness of such functionalities assessed via consulting with clinicians.
Final remarks
This article aimed to open a dialogue and discussion in our community regarding the best development practices for augmented reality image guidance systems. Further discussion taking into account a higher diversity of perspectives may create a more comprehensive and usable framework with common terminology to improve outcomes.
